Physiotherapy or Surgery?
Physiotherapy or Surgery?
If you suffer from spinal problems like a herniated disc in the back or neck, back or neck arthritis, or even slipped vertebrae (spondylolisthesis), then you need to understand whether your condition requires physiotherapy or surgery. You need to understand your condition better, know what you need, and determine if the cause of your pain is truly a herniated disc or something else, like issues with spinal curvature, muscles, or fascia.
I hope you watch the video on “Herniated Discs and MRIs” if you haven’t already, as it will explain many aspects of the examination process. If you have seen it, please read all the information on this page. If you have a problem, contact us and book an appointment, and God willing, we will be able to solve your problem.
The examination of any patient complaining of spinal pain or a herniated disc is done in three steps:
First: Symptoms
I ask the patient a series of questions, and their answers give me a preliminary idea of their condition before the physical exam. For example:
- Does the pain appear or worsen with exertion? Or is the pain constant, even without exertion? If the pain appears or worsens with exertion, it is very likely a simple case that can be resolved quickly. In this scenario, the pain is most likely not coming from the disc itself, and an imaging scan isn’t necessarily required for confirmation. It’s best to resolve the issue quickly, because the pain could become constant if you just keep taking painkillers.
- However, if the pain is constant and not related to exertion, the case is not simple and will require further examination and imaging to see if the pain is from the disc or another source. If the pain is constant and prevents the patient from sleeping, or wakes them from a deep sleep, this indicates a more difficult case that requires a more careful examination, along with a recent MRI (no older than 6 months).
This is just a small sample of the questions. There are many more that help me understand the condition better, such as: How long have you been in pain? Is the pain in your back and leg? Or just your back? Or just your leg? If it’s in the leg, is it in both legs or just one? Is there a specific position that makes the pain worse, or is it always the same? Many patients tell me, for example, “The pain gets worse when I’m sitting, and I feel better when I stand or walk for a bit.”
If the problem is in the neck, is the pain only in the neck, or in the neck and shoulder, or the neck, shoulder, and arm? If there’s arm pain, is it in one arm or both? What position makes the pain worse, and what position makes it better?
Knowing all of this helps me build an accurate picture of the condition before even looking at an MRI.
Second: The Physical Examination
After listening to your symptoms, we move on to the physical examination. I examine your movement and perform tests that help me understand the condition. For example, let’s say a patient is complaining about their lumbar spine. I ask them to bend forward towards their feet.
Based on how they bend, I form an idea about their condition. If the patient bends all the way down like in Image 1, even if there is pain during the movement or at the end of it, the important thing is that they completed the motion correctly. In this case, I can largely rule out the disc as the cause of the pain, and the problem can very likely be solved with physiotherapy.
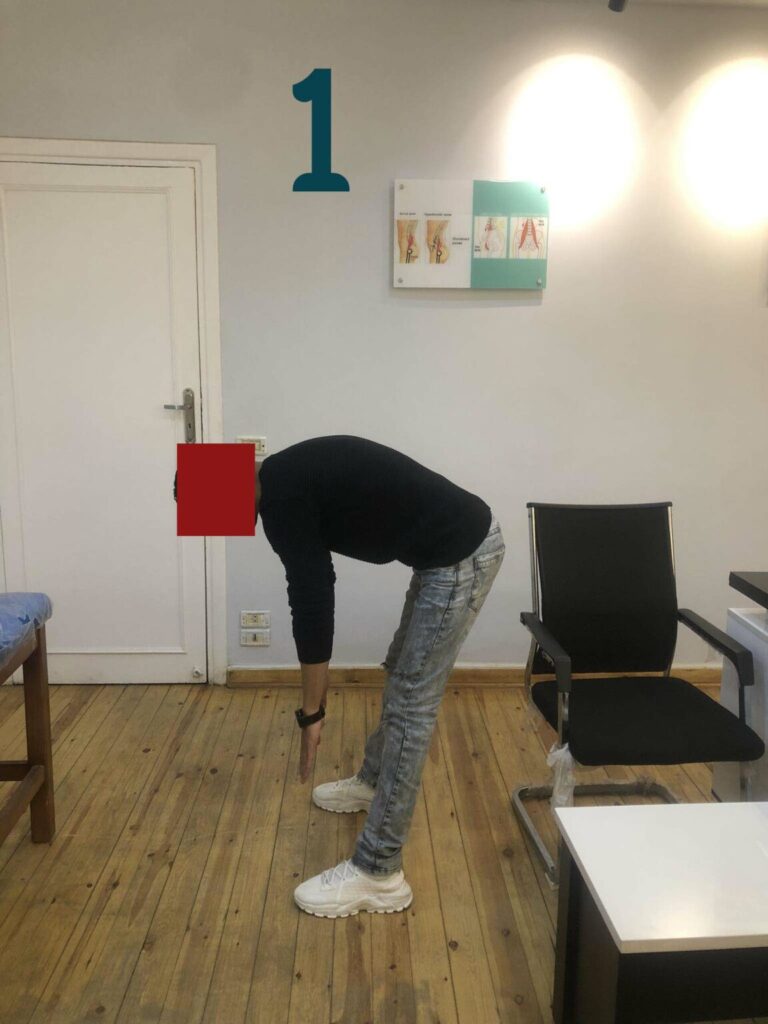
(This is an illustrative image, not a patient photo)
However, if the patient bends as shown in Image 2—unable to bend forward properly, or bending using their thoracic (upper/mid-back) spine without being able to move their lumbar (lower back) spine—then it is highly likely that a herniated disc is the cause. This requires further examination to determine if it can be resolved with physiotherapy or if it requires surgery.

Of course, bending forward is just one movement. I assess all other movements as well, such as bending backward and side-bending to the right and left. I observe whether the pain is constant in all movements, if it increases with movement, if it only appears at the end of a movement, or if it’s absent. After checking all movements, we proceed to specific tests.
This brings us to an extremely important test that all neurologists, orthopedic surgeons, and physiotherapists perform, as it is crucial in determining the patient’s condition. I ask the patient to lie on their back and raise their painful leg straight up, keeping the knee extended. If the patient can lift their leg as shown in Image 1, and the pain only occurs at the end of the motion, or even if it’s present from the start but they can still lift it, this means the problem is likely simple and, God willing, can be resolved with physiotherapy.

However, if the patient is unable to lift their leg, or can only lift it to a 30-degree angle and cannot go further, as shown in the next image, this strongly suggests the problem is a herniated disc. More tests are needed, along with a review of a recent MRI (no older than 6 months), to determine whether the path forward is physiotherapy or surgery.

And to be frank, if a patient has constant pain, is unable to bend forward, cannot lift their leg past 30 degrees, and the MRI shows a large herniated disc that has been present for a long time, there’s a high chance (around 50%) that they will need surgery. I always tell this type of patient: “We will work together for 4 or 5 sessions. If the pain begins to subside, we’ll continue with physiotherapy. If it remains the same, surgery will be the likely path.” I also want to point out that if the pain is in only one leg, there is a high chance of improvement. If the pain is in both legs, the situation is more difficult.
However, if the patient has foot drop, loss of bladder control, or sexual dysfunction, they are immediately referred for surgery. At that point, there is no need to try physiotherapy. And if surgery is the answer, I will advise you on the best surgical method for your case, as there are many different procedures, and not all are suitable for every condition.





